Overview of smart implants in orthopedics
Smart implants in orthopedics represent a deliberate fusion of mechanical design, biocompatible materials, miniature electronics, and intelligent data pathways that connect the human body with digital insight. At their core, these devices embed sensors, microprocessors, energy systems, and communication protocols within or around conventional orthopedic implants such as joint prostheses, fracture fixation devices, and spinal hardware. The intent is not merely to replace a damaged structure, but to monitor its mechanical environment, track the healing trajectory of tissues, and relay clinically meaningful information to physicians and patients in real time or near real time. This shift from static mechanical solutions to dynamic, data driven platforms holds the promise of improving accuracy in surgical planning, enabling early detection of complications, guiding rehabilitation, and supporting personalized care that adapts to how a patient heals and regains function. The language of smart implants extends beyond the metal and polymer of traditional devices to include signals, trends, and feedback loops that translate complex biology into actionable knowledge. In practical terms, a smart implant can measure load sharing across a joint, detect subtle changes in tissue stiffness as bone remodels, monitor temperature or inflammation at a surgical site, and transmit structured data to a secure database accessible to the care team. This new modality intersects with telemedicine, wearable sensors, and cloud based analytics, creating a continuum of information that can be interpreted in the context of the patient’s day to day activity, pain levels, and functional goals. The potential benefits are paired with important challenges, including ensuring patient safety, maintaining data privacy, achieving reliable wireless communication within the body, and validating clinical utility through rigorous study. Yet the overarching narrative is one of empowerment: when implants communicate, clinicians gain timely insight; when patients engage with data, they participate more actively in their own recovery; when engineers and surgeons collaborate, the design space expands to accommodate complex, real world needs rather than idealized laboratory conditions. This convergence is slowly transforming how orthopedic conditions are diagnosed, treated, and followed over the long arc of healing and functional restoration.
What makes smart implants distinct is their ability to integrate sensing, processing, and communication without compromising the fundamental goals of orthopedic devices: safety, durability, biocompatibility, and mechanical stability. The sensors embedded in these devices can range from simple strain gauges that quantify load distribution to sophisticated temperature sensors that provide early signals of infection or inflammatory response. The data produced is not an isolated stream; it is contextualized against patient specific factors such as age, comorbidities, bone quality, activity level, and prior surgical history. This contextualization often requires careful data governance, robust analytics, and clinician friendly interfaces. When effectively executed, it becomes possible to detect a loosening of a hip stem weeks before a patient experiences pain, or to identify insufficient bone integration around a fracture fixation plate before radiographic signs become obvious. The journey from sensor to decision is mediated by wireless technologies that are purpose built for medical environments, where safety and reliability are paramount, and where power management is as critical as signal fidelity. In this evolving landscape, multidisciplinary collaboration among orthopedic surgeons, biomedical engineers, data scientists, regulatory specialists, and patients themselves is essential to ensure that smart implants deliver information that is clinically meaningful and ethically sound. The result can be a more proactive paradigm of care, driven by continuous feedback rather than episodic assessments, with implications for how we measure success in orthopedic interventions.
In addition to the clinical advantages, smart implants open avenues for research and education. By capturing standardized data from real world use, researchers can interrogate questions about material performance under varied activities, the interplay between implant geometry and tissue response, and the long term implications of wear and corrosion in vivo. Educationally, surgeons can access aggregated case level data to compare techniques, outcomes, and rehabilitation strategies across patient populations, fostering learning that is grounded in evidence rather than anecdote. For patients, transparent reporting and secure access to personal performance metrics can enhance motivation during rehabilitation, helping to align daily activities with recovery milestones. The successful deployment of smart implants thus hinges on a delicate balance: maintaining the highest standards of patient safety and data integrity while unlocking the clinical and educational value that comes from continuous monitoring and knowledge sharing. The ongoing evolution of this field requires not only technical prowess but also thoughtful policy design, rigorous clinical validation, and patient centered communication that clarifies what data will be collected, how it will be used, and what benefit is expected in return for the patient’s trust and participation.
From a patient journey perspective, smart implants can shift some decisions from the clinic to the home environment. Remote monitoring capabilities enable clinicians to observe trends in healing without requiring frequent in person visits, an advantage for patients living in rural areas or facing transportation barriers. Yet remote observation also introduces questions about alert thresholds, false positives, and the workflow integration necessary to act swiftly on meaningful signals. To address these concerns, adaptive monitoring strategies are increasingly favored, where the intensity of data collection adjusts in response to the patient’s current phase of recovery, activity patterns, and any new symptoms. The human element remains central; devices aid decision making but do not replace clinical judgment. The ethical dimension of this technology includes informed consent for data collection, clarity about who has access to information, and the patient’s right to pause or opt out of certain monitoring features. In sum, smart implants embody a shift toward a more connected, data enriched surgical ecosystem, one that aspires to improve outcomes by extending the surgeon’s reach into the patient’s daily life while carefully preserving autonomy, safety, and trust.
Core technologies behind smart orthopedic implants
At the heart of smart orthopedic implants lies a triad of sensing capability, power management, and robust communication. Sensing capabilities span a spectrum from physical measurements such as strain, displacement, and load distribution to biological signals like local temperature or chemical markers that may reflect infection or tissue response. The most mature sensors in this space are mechanical strain gauges and accelerometers that quantify how a joint or fixation device experiences motion and load during everyday activities. More advanced configurations may include temperature sensors to detect fever or local heat development, impedance spectroscopy for tissue characterization, and fiber optic or optical sensors for precise, minimally invasive readings. The challenge with sensors is to ensure accuracy over the lifetime of an implant, resist drift caused by body temperature fluctuations, and remain benign with regard to tissue response and corrosion resistance. The second pillar, power, presents unique constraints because implants must operate safely for many years without frequent interventions. Batteryless designs using energy harvesting, inductive coupling, or ultra low power electronics are increasingly common. Energy harvesting can exploit body motion or metabolic processes, while inductive charging provides a practical path for recharging during follow up visits or occasional outpatient sessions. The third pillar, communication, must operate within clinical safety standards and protect patient privacy. Wireless transmission from inside the body to external receivers often relies on radio frequency protocols that are robust to the human tissue environment, with strict shielding and error correction to ensure data integrity. The data that emerges from these systems is stored or processed through secure interfaces, sometimes on the implant itself for preliminary filtering, and increasingly in cloud based platforms that support large scale analytics. Achieving reliable, low power, and biocompatible integration requires meticulous material selection, hermetic sealing to protect electronics from physiological fluids, and careful thermal management to avoid tissue heating or discomfort. The interplay between sensors, power, and communications then interfaces with software to translate raw numbers into meaningful clinical indicators, a step that is essential to turning data into decision making. The software layer must handle data normalization, artifact rejection, and patient specific baselines, all while presenting clinicians with intuitive summaries that can be acted upon within standard treatment workflows. This integration of hardware and software represents a systems engineering challenge unique to medical implants, one that demands cross disciplinary collaboration and continuous safety validation throughout the device lifecycle.
Beyond the core triad, material science and surface engineering play critical roles. Biocompatible substrates, corrosion resistant alloys, and protective coatings reduce wear and extend implant life. Surface roughness and chemistry influence tissue integration, while coatings such as hydroxyapatite or bioactive polymers can promote osseointegration around implants that interface with bone. In smart implants, the surface may also participate in sensing or energy transfer, adding another layer of complexity and opportunity. Data governance and cybersecurity are not afterthoughts but essential design considerations. Devices must be designed to resist tampering, ensure patient identity and data integrity, and comply with rigorous privacy regulations. Medical device regulations impose thorough testing regimes, including bench tests, animal studies, and human clinical trials, to demonstrate safety, accuracy of sensors, and reliability of power and communication. In practice, this means a long horizon from concept to patient use, with phased validation that establishes performance under real world conditions, including a range of body types, movement patterns, and environmental factors. The confluence of sensing hardware, energy architecture, and secure communication is the backbone of smart orthopedic implants, and it is the focal point around which clinical value is built, risk is mitigated, and patient trust is earned. In addition, the digital backbone enables integration with imaging modalities, electronic health records, and decision support systems, creating a holistic ecosystem in which the implant operates as a node within a larger network of care rather than a standalone device. This systemic perspective highlights the importance of interoperability standards, data schemas, and shared terminology so that results from different implant models, manufacturers, or care settings can be meaningfully compared and aggregated for learning and quality improvement.
Types of smart implants in orthopedic practice
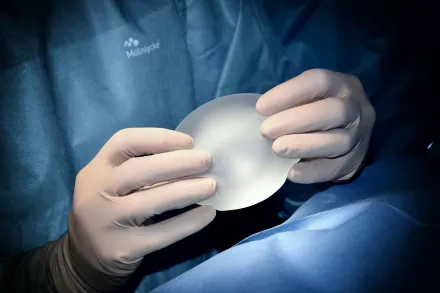
Smart implants in orthopedic practice come in several archetypes that extend the capabilities of traditional devices while preserving their essential mechanical function. Smart joint prostheses, including hips and knees, may embed sensors to measure alignment, load distribution, and interface quality with surrounding bone and soft tissues. The data from these devices can illuminate how different activities influence wear patterns, how rehabilitation protocols impact stress on components, and how patient specific factors modify the risk of loosening or osteolysis. In some designs, the prosthesis may host embedded communicators that pair with external wearable devices or clinic based consoles, enabling a synchronized view of functional status across time. Smart fracture fixation devices, such as plates and screws that monitor strain at the fixation site, offer the possibility of predicting delayed union or nonunion by illustrating how mechanical stability evolves during healing. For spinal instrumentation, smart implants can track alignment, segmental motion, and adjacent level dynamics, contributing to early detection of hardware related issues or suboptimal fusion. Another important category includes smart containment systems for tumor resections or deformity corrections, where sensors can monitor load sharing and stiffness in grafts or extendable constructs. Even dental and craniofacial implants are exploring micro sensing capabilities to inform prosthesis seating and load transfer, although these carry distinct regulatory and biomechanical considerations. The diversity of smart orthopedic implants is matched by a push toward modular designs that accommodate patient anatomy and evolving clinical questions. For instance, a smart plate might be paired with detachable sensor modules or interchangeable electronic chips that allow clinicians to upgrade the sensing capabilities without replacing the entire implant. This modularity supports customization, incremental improvement, and potentially lower long term costs by recapturing components that can be re deployed or refurbished. Yet every variant shares a common objective: to provide clinicians with a richer, longitudinal view of how an orthopaedic device interacts with the living body, so that decisions about weight bearing, rehabilitation pace, and potential interventions can be made with greater confidence and precision. The ultimate value of these types rests on the ability to synthesize data into clinically meaningful insights, while maintaining safety margins and patient comfort across dynamic daily life activities. The integration of smart implants into standard care pathways thus reflects a careful balance between innovation, practicality, patient preferences, and the realities of clinic workflows that must remain efficient and compassionate in busy care environments.
In practice, implant manufacturers and clinical teams increasingly emphasize compatibility with existing surgical techniques and patient monitoring infrastructures. The devices are designed to minimize changes to surgical steps, preserve familiar instrumentation, and fit within current regulatory frameworks so that adoption does not disrupt established care models. In some cases, smart implants are deployed with companion external devices, such as smart braces or sensor enabled assistive devices, which can collect complementary data about motion, posture, or activity levels. The synergy among these components enhances the overall picture of a patient’s functional recovery and can reveal gaps between reported symptoms and objective measurements. As clinicians gain experience with these tools, they begin to refine indications for their use, determine which patient populations stand to benefit most, and establish metrics for success that align with both clinical outcomes and quality of life. While the promise is substantial, the practice of selecting, implanting, and interpreting data from smart devices requires careful case by case judgment, transparent patient counseling, and ongoing evaluation of risk and reward in the context of evolving evidence. The field is thus characterized by a dynamic, outcome oriented approach that values both innovation and stewardship, ensuring that each smart implant adds discernible value to patient care.
Clinical applications and patient outcomes
The clinical applications of smart orthopedic implants span the continuum of care, from preoperative planning to long term surveillance. In the preoperative phase, aggregated data from smart implants and related wearables can inform surgical strategies, such as choosing implant geometry that optimizes load distribution for a given patient’s activity profile and bone quality. In the intraoperative period, sensor data can guide precise seating, alignment, and fixation, helping to tailor the procedure to the unique biomechanics of the patient. In rehabilitation, real time or near real time feedback about load sharing and joint motion can personalize weight bearing progression, assistive device use, and targeted physiotherapy. This leads to a more efficient recovery trajectory, a potential reduction in complications, and a better sense of control for patients. In the postoperative window, continuous monitoring may detect subtle signs of complications such as loosening, infection, or malalignment long before clinical signs become apparent. Early detection enables timely interventions, which can improve salvage rates, preserve bone stock, and avoid revision surgeries where possible. Over the long term, data gathered from large populations of patients can illuminate trends in implant performance under diverse living conditions, informing design improvements and personalized risk assessments. When clinicians can observe how a joint behaves under typical daily activities rather than solely under controlled laboratory tests, they gain a more robust understanding of how an implant will function in the real world. For patients, the tangible benefits include increased confidence in their prosthesis, more precise rehabilitation plans, and the potential to return to meaningful activities sooner with fewer setbacks. However, realizing these advantages requires rigorous validation, standardized reporting of outcomes, and careful attention to privacy and data sharing agreements that respect patient autonomy. The interplay of clinical science, engineering, and patient values thus defines the practical impact of smart implants on everyday life, rather than simply the novelty of technology. Clinicians who embrace these tools often adopt a balanced approach, using data intelligently to support, not replace, clinical judgment, and ensuring that any action taken from sensor alerts aligns with patient goals and evidence based medicine.
In addition to direct clinical outcomes, smart implants influence the patient experience by providing a more continuous and integrated observation of healing. Patients who understand how their implants function, and who can see progress through simple dashboards or clinician feedback, may feel more engaged in their care. Education about what the data means, how often it is updated, and how it informs decisions is essential to building trust and reducing anxiety linked to remote monitoring. At the same time, clinicians must be prepared to interpret data with nuance, considering non pathologic variations in activity levels or sensor readings that can occur due to device aging, changes in body composition, or transient illnesses. The balancing act between patient empowerment and data interpretation complexity requires streamlined interfaces, contextualized explanations, and clear pathways for escalation when sensor data suggests a potential problem. When these systems are well designed, they support a healthcare experience that is more proactive and patient centered, moving beyond episodic care toward continuous, value driven management of orthopedic conditions.
Cost considerations also shape outcome destiny. While smart implants may entail higher upfront costs related to sensors, electronics, and data infrastructure, there is a potential for downstream savings through fewer clinic visits, earlier problem detection, and optimized rehabilitation. Demonstrating cost effectiveness requires robust health economic analyses that factor in long term outcomes, device longevity, patient quality of life, and potential reductions in revision surgery rates. Accessibility, equity, and reimbursement frameworks must adapt to these evolving technologies, ensuring that the benefits of smart implants are not confined to a subset of patients who can access cutting edge care. Ultimately, the success of smart implants in improving patient outcomes will be judged not only by measurements of mechanical performance, but also by patient satisfaction, functional restoration, and the ability of the healthcare system to deliver safe and humane care at scale.
Imaging and data integration
Smart implants produce data streams that complement traditional imaging modalities such as X ray, CT, and MRI by offering functional information about load, motion, temperature, or tissue state. Integrating sensor data with imaging enhances the clinician’s understanding of the implant in the context of spatial relationships within the musculoskeletal system. For example, imaging can localize a sensor readout within a precise anatomical frame, enabling correlation of mechanical measurements with specific bones or joints. Data integration frameworks are expanding to include clinical dashboards, which synthesize sensor outputs with imaging findings and patient reported outcomes to present a coherent narrative of healing. Such dashboards may display aggregated trends over time, flag outliers that warrant investigation, and provide actionable recommendations for rehabilitation progression or imaging follow up. Interoperability standards are critical in this space, enabling data from different implant brands, sensor modalities, and patient devices to be aligned with electronic health records and decision support systems. The ultimate objective is to create an accessible, secure, patient specific view of recovery that clinicians can use to tailor treatment plans, manage complications, and communicate prognosis with patients and families. The use of artificial intelligence and machine learning in this domain is expanding, as algorithms learn to recognize patterns that correlate with successful healing, infection risk, or implant failure, while maintaining a transparent and explainable approach so clinicians can understand how the model reaches its conclusions. Balancing the power of analytics with the need to preserve patient privacy requires careful governance and encryption, ensuring that sensitive health information travels through trusted channels and remains under the patient’s control when appropriate.
In practice, data integration requires robust data governance policies, clear role definitions for clinicians and data scientists, and harmonized data dictionaries that ensure consistent interpretation across institutions. Clinicians increasingly rely on secure cloud based platforms that store de identified data for large scale research while preserving the patient’s privacy and consent. The environmental context of the data is also important; sensor readings during athletic activity, occupational tasks, or environmental stressors may influence the interpretation of healing trajectories. Therefore, contextual annotations, such as the patient’s reported pain levels or functional test results, are essential to avoid misinterpretation of raw sensor numbers. By aligning imaging, sensor data, and patient centered outcomes, healthcare teams can create a multidimensional view of recovery that informs both immediate clinical decisions and strategic planning for future care. This integrated approach supports continuous quality improvement, enabling institutions to benchmark performance, refine protocols, and accelerate the translation of insights from research into routine practice. It also invites collaboration with data governance professionals and cybersecurity experts to ensure that the expanding data fabric remains resilient against threats while providing dependable access for authorized users when needed for patient care.
Ultimately, successful imaging and data integration in smart orthopedics hinges on user friendly interfaces for clinicians, patients, and researchers. Interfaces must present complex information in a digestible form, highlighting key signals without overwhelming the user with noise. They should support rapid triage of sensor alerts, while also offering deeper dives for those who want to understand the underlying mechanics. Education and training play a critical role; practitioners require ongoing reassurance about sensor accuracy, threshold settings, and the indications for intervention based on data. When implemented thoughtfully, imaging and data integration turn sensors into practical decision support tools that augment, rather than replace, the clinical workflow. In this vision, smart implants contribute to a learning healthcare system in which every patient’s data informs improved practices for future patients, while preserving the individual’s privacy, autonomy, and well being at the center of care.
Regulatory and safety considerations
Regulatory frameworks for smart orthopedic implants are designed to ensure safety, efficacy, and ethical handling of patient data across the device lifecycle. The introduction of sensing components and wireless communication modalities introduces layers of risk that regulators examine with meticulous scrutiny. Manufacturers must demonstrate that sensors perform accurately within physiological conditions, that power systems do not generate hazardous heat, and that wireless interfaces do not create unacceptable risks of interference with other medical devices. Reliability testing becomes more complex as devices include moving parts, wear potential, and long term degradation of materials under physiological conditions. Standards organizations contribute to harmonization by providing guidelines for biocompatibility testing, sterilization validation, and electromagnetic compatibility. A rigorous risk assessment process, including failure mode and effects analysis and fault tree analysis, helps identify potential failure scenarios and guides protective design choices. Informed consent is essential because patients should understand not only the surgical procedure but also the data collection, the purpose of the sensors, the types of data generated, and how that data will be used to influence care. Regulatory oversight also extends to post market surveillance, where real world performance data are collected to monitor long term safety and to identify rare adverse events that might not appear in controlled trials. The data governance aspect includes privacy considerations, data ownership, access rights, and consent for secondary analyses or sharing within research networks. Balancing patient safety with innovation requires ongoing collaboration among clinicians, engineers, regulators, and patient representatives to adapt regulatory pathways as technology evolves while maintaining high ethical and safety standards. In the end, the regulatory environment aims to create a predictable, transparent pathway for bringing beneficial smart implant solutions to patients while avoiding undue risk and ensuring accountability for all stakeholders involved in the life cycle of the device.
Powering and longevity
Powering smart orthopedic implants is a central design constraint because devices must operate safely for many years in a location that is not easily accessible for routine maintenance. Battery powered designs offer simplicity and ease of interpretation but face end of life concerns and potential replacement procedures. Batteryless approaches, which harvest energy from body motion, temperature gradients, or ambient electromagnetic fields, are increasingly attractive because they reduce the need for surgical interventions to replace power sources. Inductive coupling and radio frequency energy transfer enable periodic recharging or wirelessly powering components without breach of the skin, provided that the exchange meets strict safety standards for tissue heating and electromagnetic exposure. Ultra low power electronics and wake–sleep strategies help preserve energy, ensuring sensors conserve power when readings are not critical. The architecture often includes on device memory for buffering data during transient outages and a secure, efficient data transmission pipeline that minimizes power use without sacrificing data fidelity. Longevity is not only about sustaining energy, but also about maintaining sensor accuracy and mechanical performance over time. Sensor drift, material wear, and changes in tissue properties can alter readings, so calibration strategies, redundancy, and diagnostic routines are embedded in the design. In addition, thermal management is a practical consideration; even small temperature elevations can discomfort patients or accelerate material degradation. Therefore, designers emphasize materials with favorable thermal conductivities, robust encapsulation, and passive cooling strategies when possible. Long term success thus depends on a holistic approach to energy management, device aging, and survival of the electronic and sensing components in the challenging physiological environment.
Interoperability related to power and communication also matters. Consistency across devices and platforms ensures that a clinician can interpret data from different implant models without learning new interfaces or sacrificing reliability. Manufacturers pursue standardized communication protocols and data formats to support scalable analytics while protecting patient privacy. In this landscape, ongoing evaluation of power budgets, battery life estimates, and failure modes informs clinical expectations and guides patient counseling. The ultimate objective is to provide dependable, continuous monitoring that does not compromise patient safety or comfort, while enabling meaningful clinical interventions when necessary. The question of cost also emerges here; while energy harvesting can reduce replacement needs, it may require sophisticated hardware that adds to upfront device costs. Decision making about power strategy thus involves a careful assessment of lifetime cost effectiveness, risk management, and patient preference, aligned with clinical goals for healing, function, and quality of life.
Biocompatibility and host response
Biocompatibility remains a foundational consideration for smart implants because the body’s response to foreign materials can influence both safety and performance. The introduction of sensors and electronics adds layers of complexity to tissue interactions, including potential inflammatory responses, fibrous encapsulation, and wear debris generation. Advanced materials science seeks to minimize adverse host responses by selecting corrosion resistant alloys, ceramic coatings, or polymeric layers that resist degradation in saline rich biological environments. Surface engineering aims to promote stable bone integration, reduce micromotion, and prevent bacterial colonization that could lead to infection. Coatings such as hydroxyapatite or biofunctional polymers can encourage osseointegration around implants that contact bone, while anti biofouling strategies help limit bacterial adherence on device surfaces. The mechanical properties of implants must also be considered to avoid stress shielding, which can lead to bone resorption and compromised fixation. Wear particles generated by articulation between implant components can provoke inflammatory cascades and osteolysis, so design and material choices emphasize low wear rates and safe byproducts. The presence of embedded electronics introduces concerns about galvanic corrosion and potential electrical interference with other devices, which is mitigated by hermetic seals, careful shielding, and rigorous testing under physiological conditions. Long term biocompatibility testing extends beyond initial safety to monitor how devices behave as patients age, and how comorbidities such as diabetes or osteoporosis influence tissue responses. The convergence of biology, materials science, and electronics in this domain requires ongoing multidisciplinary collaboration to achieve implants that not only survive in the body but actively contribute to stable biological integration and favorable healing trajectories.
Immune compatibility and patient specific factors further complicate the landscape. Genetic or environmental differences can influence wound healing rates, infection risk, and tissue compatibility with implants. Personalized assessment becomes important, where patient history, bone quality, and prior surgeries inform implant selection and sensor configuration. Infections at the implant site can dramatically alter outcomes, and smart implants may aid early detection by identifying localized temperature rises or inflammatory signals before clinical symptoms become apparent. This capability reinforces the idea that smart implants act as an early warning system, supplementing clinical vigilance with continuous monitoring. In clinical practice, the integration of biocompatibility considerations with data driven diagnostics requires thoughtful workflow design, so that sensor alerts trigger safe and appropriate responses without overwhelming clinicians with excessive information. Overall, achieving durable biocompatibility in smart orthopedic implants demands an enduring commitment to research into material science, surface engineering, immune interactions, and reliable, human centered systems that translate complex data into meaningful clinical action.
Ethical, access, and equity considerations
Ethical considerations around smart implants center on consent, autonomy, data privacy, and the equitable distribution of benefits. When a device collects data about movement, healing progress, and physiological signals, patients must have clear information about what is being recorded, how it will be stored, who can access it, and for what purposes data may be shared. Informed consent processes should explicitly address secondary uses, such as research or population level analyses, and provide options for opt out while still receiving appropriate medical care. Data privacy must comply with relevant regulations, incorporating encryption, access controls, and robust governance to prevent misuse or unauthorized dissemination of personal health information. The equity dimension is particularly salient when considering access to smart implants and the necessary data infrastructure for monitoring. High upfront costs, required follow up, and the need for reliable connectivity can exacerbate disparities if only certain populations can benefit. Policymakers and healthcare organizations must consider strategies to subsidize adoption in underserved communities, build capacity for data management, and ensure that reimbursement mechanisms align with the long term value these devices may deliver. There is also a need to be mindful of the potential for surveillance concerns, where continuous data collection might be viewed as intrusive or coercive if not managed with transparency and patient control. Fostering trust involves engaging patients in design and governance decisions, offering straightforward explanations of data use, and maintaining channels for feedback when issues arise. Ultimately, the ethical deployment of smart implants requires a patient centered, rights respecting approach that treats data as an extension of informed consent and patient welfare rather than a mere byproduct of technological progress.
From a systemic perspective, access to smart implants intersects with broader health system priorities, including workforce training, infrastructure readiness, and data interoperability. Clinicians and technicians require specialized education to interpret sensor outputs, manage device maintenance, and integrate data streams into clinical workflows. Healthcare facilities must invest in secure, scalable data platforms that can support large volumes of streaming information while remaining user friendly. Interoperability promotes equitable use by reducing the need for proprietary, siloed systems that limit data sharing. Stories of success in smart orthopedics are often tempered by the realities of cost, logistics, and the need for rigorous evidence demonstrating superior outcomes. To navigate these tensions, stakeholders should pursue transparent reporting of results, robust health economic studies, and collaborative research that includes diverse patient populations. When ethical, practical, and economic considerations are addressed in a balanced manner, smart implants can advance orthopedic care while upholding values of patient dignity, fairness, and societal trust in medical innovation.
Future directions and research challenges
The horizon for smart implants in orthopedics is shaped by a compelling mix of scientific curiosity, clinical need, and technological possibility. Researchers are exploring multi sensor fusion approaches that combine mechanical, biological, and environmental data to generate richer insights into healing, tissue response, and device performance. Advances in flexible electronics, biocompatible stretchable sensors, and energy efficient processing will enable more sophisticated sensing without compromising structural integrity or longevity. There is growing interest in integrating smart implants with regenerative medicine strategies, such as promoting bone growth or stimulating tissue healing through bioelectronic interfaces. The possibility of closed loop systems — where sensors detect a condition and a responsive actuator delivers therapy directly at the implant site — is a tantalizing prospect that could redefine recovery pathways for complex fractures or degenerative joint conditions. Nonetheless, pursuing these advances demands rigorous safety validation, constructive regulatory dialogue, and careful attention to patient outcomes. New research questions include how to optimize sensor placement for different anatomies, how to calibrate readings against varied physical activities, and how to ensure that machine learning models remain interpretable and clinically trustworthy. Another challenge is establishing standardized endpoints and data sharing agreements across institutions and manufacturers. The field must address compatibility between legacy implants and new sensor technologies to ensure that patients who initially received conventional implants can benefit from incremental upgrades without mandatory replacement. Sustainability considerations also emerge, including manufacturing footprint, material recyclability, and end of life management for devices that may remain in the body for decades. In short, the future of smart orthopedic implants lies at the intersection of deeper biological understanding, smarter materials, smarter electronics, and smarter systems of care that collectively advance patient well being while safeguarding safety, privacy, and ethical stewardship.
As the field matures, educational initiatives will be essential to translate advances into routine practice. Medical curricula, continuing education for surgeons, and hands on training for device technicians will need to adapt to the nuances of a data rich implant environment. Clinics will require new workflows to accommodate remote monitoring, data triage, and decision support while preserving the human touch that is central to compassionate care. Innovations in patient engagement will help individuals interpret their own data in meaningful ways, supporting adherence to rehabilitation plans and encouraging timely reporting of symptoms. The convergence of regulatory clarity, clinical evidence, and patient empowerment will determine how boldly smart implants can expand the boundaries of what is possible in orthopedics, while maintaining the highest standards of safety and ethical practice. By keeping focus on patient outcomes, rigorous validation, and thoughtful integration into existing care ecosystems, the field can deliver transformative improvements that are sustainable, scalable, and universally beneficial.
Practical considerations for adoption and integration
For healthcare systems aiming to adopt smart implants, practical considerations include selecting devices with clear clinical indications, ensuring compatibility with existing imaging modalities, and aligning with the institution’s data governance policies. A phased implementation strategy is prudent, beginning with pilot programs that focus on well defined patient cohorts, precise clinical questions, and measurable outcomes. Training and support for surgeons, nurses, and rehabilitation therapists are crucial to maximize the value of these devices and to minimize workflow disruptions. Data pipelines should be designed with redundancy, security, and patient privacy at the forefront, including clear consent processes, access controls, and transparent data usage policies. Reimbursement planning is also essential, requiring collaboration with payers to establish coverage for device related monitoring and associated follow up. In parallel, patient education materials should explain what data is collected, how it is used, and what benefits might be expected, as well as potential risks and the steps taken to mitigate them. A patient centered approach to implementation emphasizes shared decision making, where individuals understand the trade offs between conventional implants and smart variants, including expectations for follow up, possible alerts, and the role of remote monitoring in their care plan. Finally, continuous evaluation is important: collecting real world evidence, monitoring safety signals, and publishing findings helps ensure that the adoption of smart implants translates into tangible improvements in function, pain relief, and quality of life for a broad patient base rather than remaining a niche capability. By weaving together clinical judgment, engineering excellence, and patient collaboration, adoption can be both effective and ethically grounded, ultimately expanding the reach and impact of orthopedic care in the decades to come.










