The Role of Robotics in Minimally Invasive Procedures
In the medical landscape, minimally invasive procedures have transformed patient care by combining precise targeting with reduced trauma. The integration of robotics into this domain represents a synthesis of advanced engineering, sophisticated control systems, and clinical expertise. The term robotics in surgery encompasses devices that extend the capabilities of the human surgeon, offering precision, steadiness, and enhanced visualization. Across specialties, robotic assistance is being used to perform a spectrum of interventions, from delicate dissections in narrow operative corridors to highly accurate resection and reconstruction tasks. The flow of information between the surgeon and the machine is orchestrated through a carefully designed interface that translates intention into motion while maintaining safety and adaptability. This article surveys the multifaceted role of robotics in minimally invasive procedures, tracing its historical roots, analyzing the core technical principles, describing current platforms, and outlining future directions. It emphasizes how robotic systems can complement human skill rather than replace it, and it discusses the practical implications for training, patient outcomes, and health systems while acknowledging the ethical and logistical considerations that accompany widespread adoption.
Historical perspective on minimally invasive surgery and early robotics
The evolution of minimally invasive surgery began with a shift from large, traumatic incisions toward targeted access through small ports and natural orifices. Surgeons sought to minimize tissue damage, reduce infection risk, and shorten recovery times while maintaining or improving oncologic and functional outcomes. Early robotic ideas emerged from the desire to overcome tremor, magnify visualization, and enable more precise instrument control than could be achieved with traditional laparoscopy. In the late twentieth century, experimental robotic systems demonstrated that teleoperation—where the surgeon’s movements are transmitted to robotic instruments—could enhance steadiness and accuracy in confined spaces. The pivotal transition from experimental prototypes to clinically deployed systems occurred with the advent of master-slave configurations, where the surgeon manipulates a console while robotic manipulators execute precise actions within the patient. The most notable milestone was the introduction and subsequent refinement of a widely adopted master-slave platform that earned broad clinical acceptance and regulatory clearance, marking a turning point in how surgeons approached complex procedures. Implementation of these systems was accompanied by rigorous training, careful patient selection, and a framework for evaluating outcomes that emphasized safety, precision, and reproducibility across diverse surgical domains. The historical arc also included iterative improvements in ergonomics, instrument articulation, imaging, and control responsiveness, which collectively laid the groundwork for modern robotic-assisted minimally invasive procedures.
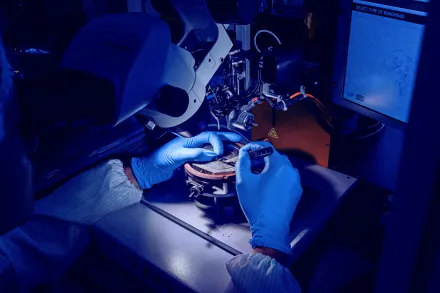
Technical foundations of surgical robotics
At the core of robotic assistance in surgery lies a set of technical principles that harmonize surgeon intent with robotic execution. A typical master-slave system translates the surgeon’s hand motions into precise movements of remotely controlled instruments that operate inside the patient. This arrangement introduces a level of precision and stability that surpasses manual manipulation, particularly in tasks requiring fine dissection, precise suturing, or steady retraction within narrow corridors. The control loop often includes scaling and filtering to optimize tactility and responsiveness, along with sophisticated kinematic models that interpret instrument pose and orientation. Visual feedback, usually through high-definition three-dimensional imaging, provides depth perception and spatial awareness that are essential for safe navigation around critical structures. Haptic feedback, although not universally integrated, aims to restore a sense of touch by conveying force or tactile cues back to the surgeon, thereby enhancing perception of tissue properties and instrument interactions. In parallel, a reliable imaging chain combines real-time endoscopic views with preoperative data, enabling image-guided decisions and alignment with planned trajectories. Safety mechanisms, including instrument collision avoidance, encounter with tissue, and emergency stop capabilities, are embedded in the software and hardware stack to protect patients during complex maneuvers. Finally, robust communication protocols and latency management ensure that the human operator’s commands translated through the system remain synchronous with the surgical scene, minimizing delays that could affect precision or judgment during delicate steps.
Robotic platforms and their evolution
The landscape of surgical robotics has expanded far beyond the earliest master-slave configurations to include a variety of platforms tailored to different specialties and tasks. The most widely recognized system, often cited in discussions of modern robotic surgery, introduced a high-precision, multiport approach that enables triangulation and improved access to deep anatomy. Over time, engineers introduced enhancements such as better instrument articulation, improved visual optics, and integrated workflow features that streamline docking, setup, and intraoperative transitions. In parallel, specialized platforms emerged to address particular domains, including orthopedics where robotic assistance assists alignment and planning for implants, and otolaryngology where endoluminal approaches benefit from flexible instruments and enhanced visualization. The evolution also includes efforts to miniaturize components, extend range of motion, and incorporate imaging modalities that support tissue characterization and real-time decision making. Contemporary systems frequently incorporate modular architectures, enabling surgeons to select instrument arms, camera configurations, and control interfaces that suit the procedure, patient anatomy, and surgeon preference. This diversity reflects a broader trend toward customization, where the choice of platform is guided by clinical objectives, patient safety, and the anticipated biomechanical demands of the operation rather than a one-size-fits-all paradigm.
Impact on patient outcomes and clinical performance
Robotic assistance in minimally invasive procedures has been associated with several clinically meaningful advantages, particularly in complex operations or anatomically challenging regions. Improved visualization and instrument dexterity can translate into more meticulous tissue handling, reduced unintended tissue trauma, and the ability to perform precise suturing in confined spaces where human hands would be less stable. Studies in various specialties have reported reductions in blood loss, clearer delineation of critical anatomic planes, and enhanced accuracy of anatomic reconstructions. Shorter hospital stays and faster postoperative recovery are frequently cited outcomes, though these benefits can vary depending on procedure type, patient characteristics, and the surgeon’s experience with the robotic system. Importantly, robotics can expand the range of patients eligible for minimally invasive approaches, offering feasible options in anatomies or clinical scenarios where conventional laparoscopy would be less effective or more challenging. However, the relationship between robotic assistance and outcome improvements is nuanced; success hinges on careful patient selection, meticulous intraoperative technique, and a robust postoperative care pathway. The ongoing accumulation of multicenter data, standardized outcome metrics, and long-term follow-up are essential to translate early promise into consistently demonstrated value across health systems and patient populations.
Training, adoption, and the surgeon-robot collaboration
Adopting robotic systems in the clinical setting requires a comprehensive approach that extends beyond installation and maintenance. Training programs emphasize a progression from simulated environments to supervised operating room experiences, with defined milestones that ensure the surgeon develops competence in instrument handling, spatial navigation, and decision making under the constraints of robotic interfaces. Simulation platforms, including virtual reality environments and physical task trainers, allow trainees to practice suturing, knot tying, and dissection with feedback on precision and efficiency before entering the actual operative field. The learning curve is influenced by the complexity of the procedure, the surgeon’s prior experience with laparoscopy, and the team’s familiarity with the robotic workflow. Team dynamics are crucial, as anesthesia, nursing, and instrument technicians must synchronize with the surgeon’s pace and use of advanced features such as camera control, instrument exchange, and console-based decision support. Ergonomic considerations for surgeons, who operate for extended periods at a console, include posture, console design, and cognitive workload management to sustain performance across lengthy cases. Institutions that invest in structured curricula, credentialing pathways, proctoring, and continuous skills assessment often observe more rapid integration of robotics into routine practice with safer patient care. The culture of adoption also encompasses patient education, consent processes that clearly articulate what robotic assistance entails, and transparent discussions about expectations, potential benefits, and residual risks.
Imaging, visualization, and sensory feedback in robotic surgery
The visualization ecosystem in robotic surgery emphasizes fidelity, depth perception, and real-time information that supports precise tissue discrimination. High-definition three-dimensional imaging, when coupled with magnification and depth cues, affords improved appreciation of subtle planes and tissue characteristics that guide dissection and suturing. Some platforms integrate advanced imaging modalities such as fluorescence imaging to highlight vascular structures or tumor margins, providing additional layers of information during critical steps. Augmented reality concepts are explored as a means to superimpose preoperative planning data onto the intraoperative view, helping surgeons align their actions with an overarching strategy. While visual enhancements substantially aid performance, there remains a focus on balancing information richness with cognitive load, ensuring that sensory feedback remains intuitive rather than overwhelming. In certain systems, attempts to reintroduce tactile sensation through haptic feedback aim to convey tissue stiffness, pliability, and resistance to instrument contact. The ongoing development of sensory modalities—from force sensing in the instrument tips to predictive modeling of tissue response—seeks to create a more natural and reliable feed for the surgeon, which can translate into greater precision and safer tissue handling across diverse procedures.
Autonomous and semi-autonomous robotics in the operating room
Autonomy in the surgical domain is pursued in a careful, incremental fashion that preserves the surgeon as the ultimate director of the procedure. Semi-autonomous functions may undertake repetitive or highly precise tasks, such as tremor suppression, automated suturing, or precise alignment of implants, under direct human oversight. Autonomous modes are typically constrained by safety boundaries, strict procedural scripts, and real-time monitoring to prevent unintended movements. The promise of autonomy lies in reducing surgeon fatigue, standardizing critical steps, and enabling complex tasks to be executed with high repeatability across cases. Yet, the deployment of autonomous capabilities demands extensive validation, rigorous risk assessment, and comprehensive regulatory oversight to ensure patient safety. The collaboration between human judgment and machine execution is often framed as a complementary partnership, where the robot handles technical precision and throughput while the surgeon concentrates on strategic planning, intraoperative decision making, and nuanced adjustments required by patient-specific anatomy. Ethical and professional expectations increasingly emphasize transparency about the limitations of autonomous features, clear consent for their use, and continuous oversight to preserve the primacy of human clinical judgment in surgical care.
Challenges and limitations of robotics in minimally invasive procedures
Despite the promise, robotic systems face a range of practical and conceptual challenges. The costs associated with purchase, maintenance, and disposable instruments can be substantial, prompting careful economic analyses that weigh upfront investment against long-term value. Operational considerations, such as docking time, instrument exchange, sterilization logistics, and system downtime, influence case throughput and scheduling. The tactile feedback gap—tactile sensation that surgeons rely on in open or conventional laparoscopic surgery—remains a persistent limitation in many platforms, affecting tissue characterization and force control. Instrument design constraints, including limited degrees of freedom in certain configurations and restricted reach in challenging anatomies, can limit the applicability of robotic assistance in some procedures. Additionally, the integration of robotics into an existing surgical workflow requires robust IT infrastructure, reliable data management, and standardized maintenance routines to minimize interruptions. Regulatory considerations, safety concerns, and ongoing surveillance for adverse events are essential components of responsible adoption. Finally, the learning curve for institutions deploying robotics implies that patient outcomes in the early experience phase may differ from long-term results, underscoring the need for structured training, mentorship, and continuous quality improvement initiatives across teams and centers.
Ethical and patient-centric considerations
As robotic technologies become more prevalent, ethical questions surrounding access, equity, and patient autonomy come to the forefront. Ensuring that benefits are shared broadly across patient populations requires strategic planning to avoid disparities in access to advanced surgical options. Informed consent processes must articulate the role of robotic assistance, potential risks, and alternative approaches in language that is clear and comprehensible to patients and families. Data privacy concerns arise because robotic systems generate and transmit identifiable information about surgical performance, workflow, and patient condition. Safeguards around data ownership and usage must be established, along with transparent policies for sharing de-identified information for research and quality improvement. The balance between automation, surgeon autonomy, and patient safety requires ongoing ethical oversight, including independent monitoring of new capabilities and continuous alignment with professional standards of care. Clinicians and researchers must also consider long-term implications for training pipelines and workforce dynamics, ensuring that technological progress does not inadvertently create gaps in clinical expertise or future readiness among surgeons and support teams.
Future directions and disruptive trends in robotic minimally invasive surgery
The horizon of robotic surgery is shaped by a convergence of advances in materials science, artificial intelligence, and data-driven decision support. Soft robotics promises compliant, adaptable grippers and safer tissue interactions in delicate procedures, while continuum robots offer enhanced flexibility to navigate tortuous anatomical pathways. Advances in sensing, including force feedback, tissue property mapping, and real-time tissue classification, are expected to enrich intraoperative decision making. The integration of machine learning models trained on large datasets of surgical cases holds potential for predictive guidance, automated planning, and real-time error detection, augmented by surgeon oversight to maintain clinical intent and safety. Single-port and natural orifice approaches foster more cosmetically favorable outcomes and further reduce tissue trauma, while multiport configurations continue to evolve with smarter docking and streamlined instrument exchanges. The role of augmented reality and data visualization is likely to expand as preoperative plans are synchronized with live intraoperative cues, enabling a more intuitive mapping between strategy and execution. In pediatric and congenital populations, lightweight, compact robotic systems could extend the reach of minimally invasive techniques while maintaining stringent safety standards. As technology matures, collaborations between engineers, surgeons, and biologists will drive the creation of hybrid systems that blend imaging, sensing, and actuation in new ways, supporting a future where robotic assistance becomes a natural extension of surgical judgment and dexterity.
Clinical integration across specialties and case examples
Across specialties such as urology, gynecology, general surgery, thoracic surgery, and otolaryngology, robotic assistance is being tailored to the unique anatomic challenges and procedural goals of each field. In urology, precise dissection around delicate neurovascular structures and meticulous suturing of reconstructive elements contribute to functional preservation alongside oncologic control. Gynecologic surgeons exploit enhanced visualization to optimize minimally invasive hysterectomies, myomectomies, and complex pelvic reconstructions, balancing hemostasis with tissue preservation. General surgeons apply robotics to complex hernia repairs, colectomies, and intricate dissections that benefit from improved triangulation and stable hand control. In thoracic surgery, robotic platforms enable precise pulmonary resections, lobectomies, and mediastinal explorations with enhanced access to posterior or apical regions. Otolaryngology, with its tight spaces and critical structures, leverages flexible instrumentation and refined visualization to perform endoscopic resections and microdissections that would be challenging with traditional approaches. Each specialty contributes to a growing body of case-level evidence, experiential knowledge, and refined best practices that collectively elevate the standard of care. The cross-pollination of techniques and outcomes across disciplines accelerates the maturation of robotics, encouraging shared learning and standardized protocols that optimize safety, efficacy, and patient satisfaction across the surgical spectrum.
Economic considerations and health system impact
Adopting robotic technologies entails a comprehensive assessment of cost, value, and system-wide implications. Initial capital expenditure for the robotics platform, ongoing maintenance contracts, and instrument per-case costs must be weighed against potential savings from shorter hospital stays, reduced postoperative complications, and faster return to normal activities. Financial analyses often examine the learning curve, throughput, and instrument utilization rates to estimate amortization periods. Operational efficiency, including docking times and turnover, can influence unit costs, and investments in training and simulation may yield longer-term gains in safety and productivity. Health systems also grapple with procurement strategies, including tiered adoption across centers of excellence versus widespread dissemination, and considerations about equitable access for patients in diverse geographic and socioeconomic contexts. Reimbursement frameworks, payer policies, and outcome-based payment models increasingly shape decisions about where and how robotics is deployed. Ultimately, the economic reality of robotic minimally invasive procedures depends on a careful balance of upfront investment, ongoing operating costs, clinical benefits, patient expectations, and organizational readiness to integrate technology into complex care pathways.
Regulatory landscape and safety assurance
Regulatory oversight ensures that robotic systems meet stringent standards for safety, effectiveness, and quality. Competent regulatory agencies assess preclinical data, clinical trial results, labeling, and the ability of devices to perform as intended under a range of conditions. Post-market surveillance, adverse event reporting, and device recalls remain essential components of maintaining trust in complex medical technologies. Standards organizations contribute by developing interoperability guidelines, performance benchmarks, and test protocols that facilitate consistent evaluation across platforms and evolving generations of devices. Safety assurance encompasses a lifecycle approach that covers design validation, risk assessment, sterilization practices, software updates, and cybersecurity measures to protect patient data and device integrity. Training requirements, credentialing processes, and institutional governance further strengthen safety by ensuring that operators and teams bring appropriate expertise to the operating room. As robotic technologies advance, ongoing collaboration among clinicians, engineers, regulators, and patients will continue to shape a robust framework that supports innovation while upholding the highest levels of patient safety and quality of care.
In the evolving field of minimally invasive robotic surgery, the synergy of precision engineering, intuitive human control, and rigorous clinical practice defines a path toward safer, more effective interventions. The journey from early prototypes to integrated surgical ecosystems reflects a persistent commitment to improving outcomes while respecting the complexities of human anatomy and the realities of clinical care. As researchers and clinicians explore new materials, smarter algorithms, and adaptive imaging, the role of robotics is likely to expand beyond current boundaries, enabling surgeons to perform tasks that were once deemed impractical or unattainable. The ultimate measure of success will be a consistent enhancement of patient experiences, a reduction in procedure-related risks, and a healthcare landscape that makes advanced surgical options accessible to a broad and diverse population. In this continuing evolution, the central aim remains clear: to empower surgeons with tools that amplify skill, enhance safety, and accelerate recovery, while maintaining the compassionate, patient-centered core of medical practice.










