Understanding the evolving landscape of elder care and rehabilitation
In recent years the field of physical therapy for older adults has undergone a quiet but profound transformation driven by advances in robotics and intelligent sensing. As populations age, the demand for safe, effective, and scalable rehabilitation options grows, and robotics offers a set of tools that complement traditional hands on therapy without replacing the crucial judgment of skilled clinicians. Robotic systems provide repeatable, precise, and engaging experiences that can extend the reach of therapy beyond what a patient might accomplish with a single therapist in a single session. The demographic shift toward longer life expectancies means therapists are increasingly asked to design programs that accommodate varying levels of independence, chronic conditions, and fluctuating energy levels. In parallel, the cadence of care has changed as families and health systems seek solutions that reduce risk of injury, improve adherence to exercise regimens, and accelerate recovery when recovery is possible. It is within this context that robotics emerges not as a replacement for compassionate care but as an amplifier of therapeutic potential, helping elderly patients move more confidently, with greater safety, and with more data to guide future sessions.
The core idea: robotics as an ally in moving with intention
Robotics in elderly physical therapy is built on a simple but powerful premise: well designed robotic systems can guide movement, support joints, and provide real time feedback in ways that reinforce correct motor patterns. When a patient with osteoarthritis or after a stroke practices standing up or stepping forward, a robotic interface can sense subtle shifts in weight, detect compensatory strategies, and gently guide the limb through a sequence that promotes proper alignment. This does not diminish the therapist’s role; instead it frees the clinician from counting repetitions and monitoring basic safety so that attention can be directed toward correcting technique, adjusting goals, and personalizing the experience to a patient’s daily life. The result can be a therapy that feels more like a collaborative dance between human insight and machine assistance, where the robot handles the mechanics and the clinician attends to motivation, emotional engagement, and meaningful outcomes.
Categories of robotic systems and how they fit into therapy
Within rehabilitation, several broad categories of robotic systems address different therapeutic goals. End effector devices guide movement by controlling the end point of the limb, such as the foot or hand, and are used to practice repetitive tasks like gait training or reaching. Exoskeletons and wearable loks provide support along multiple joints, enabling patients with weakness to perform activities that might be impossible unaided, while gradually reducing assistance as strength improves. Robotic gait trainers can assist with walking patterns on a treadmill or overground surface in a controlled manner, allowing therapists to adjust speed, stride length, and temporal parameters with precision. Robotic assistive devices such as intelligent canes or plate-like interfaces can deliver just enough support to enable safe practice of dynamic activities, while haptic feedback and sensory cues enhance proprioception and body awareness. Additionally, telepresence robotics can connect patients with remote therapists for guided sessions, enabling continuity of care when in-person visits are limited. Each category serves a distinct purpose, and the most effective therapy program often integrates several of these modalities in a cohesive plan tailored to the individual patient’s functional goals and home environment.
Safety first: designing for protection and trust
Safety is the cornerstone of any robotic approach to elderly rehabilitation. Systems are designed with multiple layers of protection, from soft, compliant actuation and passive restraints to real time monitoring of vital signs and posture. Clinicians screen candidates to ensure that cognitive status, sensory function, and medical stability align with the demands of a robotic program. In practice this means careful calibration of assistance levels so that the patient remains in control, with the robot stepping in only where needed to prevent compensatory patterns that could lead to injury. Transparent interfaces, intuitive controls, and clear feedback help build trust between patient and device, which in turn encourages consistent participation. Safety protocols extend beyond the device itself to include proper cleaning, maintenance, and staff training, ensuring that environments where robotics is used remain calm, clean, and supportive for frail individuals who may be more susceptible to infections or falls.
Enhancing motivation and adherence through engaging feedback
One of the most meaningful benefits of robotics in elderly therapy is the way technology can enhance motivation and adherence. Real time feedback shows patients how their movements compare to a target pattern, and progress metrics enable families and clinicians to celebrate incremental improvements. Gamified elements and engaging visual displays can transform repetitive exercise into purposeful activity, reducing fatigue and increasing willingness to participate in sessions. The social dimension matters as well; when a patient senses that a therapist is reviewing objective data and responding with a personalized plan, it reinforces trust and motivation. This shift from rote repetition to meaningful practice helps patients stay engaged over longer periods, which is essential for neuroplastic changes and regaining functional independence. At the same time, data captured during sessions supports clinicians in adjusting difficulty, pacing, and goal setting, ensuring that therapy remains aligned with evolving capabilities and daily routines.
Impact on gait and balance: improving stability with guided practice
Balance and gait are central concerns for many elderly individuals and a common target of physical therapy. Robotic devices designed to assist with standing and stepping enable patients to practice a variety of challenging tasks in a controlled environment. By modulating support and resistance, therapists can encourage step symmetry, cadence normalization, and an upright posture that reduces the risk of falls. For patients with Parkinsonian gait or post-stroke hemiparesis, calibrated robotic assistance can help retrain walking patterns while reducing the energy cost of movement. The consistent, repetitive practice made possible by robots complements manual techniques and can accelerate the reeducation of neuromuscular pathways. While progress may be gradual, the reliability of robotic systems means sessions can be extended with less fatigue and fewer interruptions, contributing to the overall effectiveness of the rehabilitation program and allowing patients to experience meaningful improvements in daily mobility.
Upper limb rehabilitation: aiding reach, grip, and dexterity
The role of robotics in supporting upper limb therapy for elderly patients encompasses a range of tasks such as reaching, grasping, and manipulating objects. Robotic gloves or end effector devices can assist finger and wrist movements with adjustable assistance levels, enabling patients to practice reaching across planes, performing object transfer tasks, and reestablishing coordinated arm control. For individuals recovering from stroke or dealing with degenerative conditions, such devices provide safe, repetitive practice that fosters neuromotor recovery while preserving hand health. The ability to quantify grip strength, movement smoothness, and range of motion creates a data-rich environment for clinicians to tailor interventions, monitor progress, and respond quickly to plateaus or new functional goals. Importantly, upper limb robotics can be integrated with functional tasks that resemble activities of daily living, making therapy more relevant and easier to translate into home practice.
Home-based robotics: extending therapy beyond the clinic walls
Robotics is increasingly enabling home based therapy programs, which is especially beneficial for elderly patients who face transportation challenges or live in remote areas. Portable or modular robotic systems can be introduced in a patient’s living space, providing guided practice without the daily transport to a clinic. Calibration and remote oversight remain critical; therapists can configure home programs, review captured data, and adjust the level of assistance from afar, maintaining continuity of care while supporting independence. Home based robotics also plays a role in caregiver education, offering step by step guidance for safe assistance and ensuring that the patient remains within an appropriate exercise envelope. The broader implication is a shift from episodic care to ongoing, data informed rehabilitation that aligns with real life routines and environmental contexts, which helps embed healthier movement habits into everyday activity.
Interoperability with clinical workflows and data analytics
For robotics to be valuable in elderly rehabilitation, it must integrate smoothly with clinical workflows and existing health information systems. Data from robotic systems can be embedded into electronic health records, enabling clinicians to track performance trends, adjust care plans, and coordinate with physicians, caregivers, and community services. Standardized metrics such as movement smoothness, range of motion, reaction time, and stability scores facilitate comparisons across patients and time. This data driven approach supports evidence based practice and can help facilities quantify outcomes at the program level, informing decisions about resource allocation, therapy intensity, and staffing needs. Seamless integration also reduces documentation burdens for therapists, enabling them to focus more on direct patient interaction and the nuanced decisions that require clinical judgment while the robots handle standardized data collection and error prevention.
Individualization: personalizing therapy to the lifelong story
Every elderly patient has a unique medical history, set of goals, and daily life requirements. Robotic systems excel when they are tuned to these individual narratives rather than applied as a one size fits all solution. Personalization can involve adjusting the degree of assistance to gradually shift responsibility to the patient, selecting movement tasks that resemble activities the patient values, and incorporating real world contexts such as kitchen or garden tasks into practice. Clinicians partner with patients to define meaningful targets, whether the objective is to regain independence with morning routines, to improve balance for safe ambulation around the home, or to participate in a beloved activity like social dances or gardening. When robotics is used with a patient centered mindset, the technology becomes a means of supporting autonomy rather than a clinical obligation, and it respects the patient’s preferences, routines, and pace of change.
Clinical decision making and progression: when to escalate or scale back
The progression of a robotic therapy program is guided by a combination of objective data and clinical observation. Therapists watch for signs that a patient is ready for increased challenge, such as improved movement quality, reduced effort, and increased confidence in performing tasks without manual support. Conversely, signs of fatigue, unsafe compensations, or diminishing engagement may trigger adjustments to reduce difficulty or pause certain activities. Because robotic systems can provide precise measurements and repeatable conditions, clinicians gain a clearer understanding of when progress truly reflects genuine motor learning and when it may be the result of temporary factors such as mood or pain. This nuanced decision making is essential to avoiding overtraining and ensuring that every session builds toward functional goals that matter to the patient’s daily life.
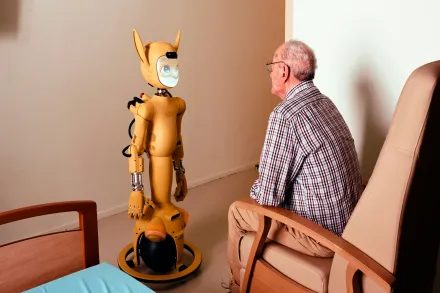
Ethical considerations and equitable access
As robotics becomes a more prominent element of elderly rehabilitation, ethical questions about access, equity, and the cultural acceptability of machine assisted therapy arise. Not all facilities have the resources to acquire sophisticated robotic systems, and not all patients are comfortable with technology. Programs must address disparities in access, provide transparent information about risks and benefits, and ensure that the introduction of robotics does not widen existing gaps in care. Clinicians should emphasize informed consent, respect patient autonomy, reassure patients about data privacy, and tailor explanations to individual education levels. When implemented thoughtfully, robotic assisted therapy can democratize rehabilitation by offering scalable, high quality therapy options that complement skilled human care rather than replacing it, especially for patients who require extended or intensive practice to achieve meaningful gains.
Training and education for therapists, patients, and families
The successful deployment of robotics in elderly physical therapy depends on comprehensive training for clinicians, robust onboarding for patients, and clear guidance for family members involved in home practice. Therapists benefit from continuing education that emphasizes device physics, safety protocols, data interpretation, and strategies for maintaining therapeutic rapport while using machines. Patients gain confidence when they understand how the device works, what the targets are, and how progress will be measured. Families and caregivers need practical instruction on device setup, cleaning routines, and how to support but not micromanage practice sessions. Educational materials should be accessible, culturally sensitive, and designed to reinforce the sense that the technology is a partner in health, not an unfamiliar hazard. High quality training reduces the learning curve, enhances safety, and supports sustained engagement with rehabilitation programs that rely on robotic assistance.
Cost considerations and value proposition
Buying and maintaining robotic systems involves upfront investment and ongoing costs, including service, software updates, and consumables. However, the value proposition extends beyond the sticker price. By enabling more efficient therapy sessions, enabling home based practice, extending the period of safe engagement in challenging tasks, and reducing falls risk, robotics can contribute to shorter rehabilitation timelines, fewer hospital readmissions, and improved quality of life. Decision makers weigh these factors against budget constraints, workforce availability, and the willingness of staff and patients to embrace new modalities. A thoughtful implementation plan can maximize return on investment by prioritizing devices with strong safety profiles, reliable data outputs, and proven benefits in improving functional independence for older adults.
Case narratives: real world implications for daily life
Consider a patient who has experienced a mild stroke and struggles with unilateral weakness that limits daily activities. A robotic gait trainer may help the patient practice stepping with symmetry while the therapist monitors alignment and muscle activation. Over weeks, the patient notices improved confidence in standing, smoother transitions from sit to stand, and a greater ability to participate in family activities that were previously too tiring. Another example involves a person with advanced osteoarthritis who benefits from an assistive robotic exoskeleton that supports knee and hip joints during weight bearing tasks. The patient can practice controlled weight shifts and controlled limb movements with less pain and greater confidence, gradually reclaiming the capacity to perform basic tasks such as dressing and shopping with less assistance. In each story the robot does not operate in isolation; it acts as a scaffold that allows the therapeutic alliance to be more effective, more precise, and more attuned to the patient’s lived experience.
Research avenues and the path forward
Academic and clinical researchers continue to investigate how robotic systems influence outcomes across different conditions common in elderly populations. Studies explore how machine learning can adapt assistance in real time based on movement quality, fatigue levels, and pain indicators. Other lines of inquiry examine how multimodal feedback, combining visual, auditory, and tactile cues, can augment motor learning and retention. Trials also assess long term effects on independence, caregiver burden, and health care utilization, such as emergency visits and hospital length of stay. Beyond clinical outcomes, investigations examine the social dimensions of robot mediated therapy, including how patients perceive autonomy, trust in technology, and the perceived dignity of participating in a highly structured therapy that is guided by a machine. The evolving evidence base will continue to shape guidelines, reimbursement policies, and the design of devices that align with the values and goals of elderly patients and their care teams.
Facility design, workflow integration, and practical deployment
Factories, clinics, and senior living communities looking to adopt robotics must consider how devices fit within physical spaces, cleaning protocols, and daily routines. Adequate room for safe device operation, clear pathways to avoid congestion, and comfortable waiting areas contribute to a favorable experience for patients and staff alike. Scheduling becomes an art as therapists balance time with robotic sessions and manual therapy, ensuring that each patient receives sufficient exposure to both modalities. Maintenance plans should specify routine checks, calibration procedures, and rapid response processes for any device alarms. When thoughtfully integrated into the facility's care philosophy, robotic systems can complement the skills of therapists, reduce the likelihood of manual fatigue, and create a sustainable model for delivering high quality rehabilitation to large numbers of elderly patients while maintaining a patient centered, compassionate approach.
Caregiver perspectives and family involvement
Families often play a pivotal role in supporting rehabilitation outside the clinic. Robotics can empower caregivers by providing clear instructions, monitoring progress, and enabling safe home practice. For example, a robotic device configured to assist with daily living tasks can help an elder patient practice safe transfers from bed to chair, or promote stability during ambulation around the house. Caregivers benefit from objective progress reports that illustrate improvements over time, helping to set realistic expectations and celebrate milestones. At the same time caregivers may have concerns about managing technology, data privacy, and the potential loss of personal touch in care. Transparent conversations, shared goals, and ongoing education help align expectations and ensure that technology serves as a conduit for increased independence rather than a source of frustration or anxiety.
Ethical resonance: dignity, autonomy, and respect in robotic assisted therapy
The ethical landscape surrounding robotic assisted therapy centers on how technology shapes the patient’s sense of dignity and agency. Devices should be designed to preserve privacy, minimize intrusion, and offer meaningful choices to each patient about how and when to engage with practice sessions. Clinicians must remain sensitive to cultural values, personal preferences, and the meaning that independence holds for each individual. Robots should not be seen as substitutes for human contact but as tools that enable more respectful, collaborative, and empowering care. As the technology matures, it is essential that stakeholders—patients, families, therapists, administrators, and policymakers—continue to examine the balance between automation and human connection to ensure ethical and person centered care for aging populations.
Cross-disciplinary collaboration: forging partnerships for better outcomes
Robotics in elderly rehabilitation thrives when clinicians work with engineers, data scientists, and human factors experts to design, test, and refine devices. Collaborative teams can translate clinical insights into device features that address real world needs, such as intuitive interfaces, safe fail safes, and robust data reporting. This cross-disciplinary approach accelerates iterative improvements, ensures devices align with patient goals, and fosters innovation that remains grounded in practical therapy context. In turn, engineers benefit from direct clinical feedback that sharpens usability and reliability, reducing the risk of delays or misalignment with therapeutic objectives. The resulting ecosystem makes it possible to push the boundaries of what is feasible in elderly rehabilitation while keeping patient safety and comfort at the forefront.
Patient stories and the human heartbeat behind the technology
Beyond metrics and study results, the enduring impact of robotic assisted therapy is felt in patient narratives. A grandmother who regained confidence to walk to the mailbox without fear of falling, a neighbor who could return to volunteering at a community center, or a father who could stand long enough to share dinner with his family—all these stories reflect the life changing potential of technology used with care and empathy. Each story demonstrates that robotics can offer precise, repetitive, and safe practice, while the therapist provides encouragement, empathy, and meaning. When patients experience these tangible improvements in daily life, technology ceases to be an abstract concept and becomes a partner in preserving independence, dignity, and the ability to participate in the activities that give life purpose.
Policy, funding, and the road to broader access
Wider adoption of robotic enabled rehabilitation depends on supportive policy frameworks and sustainable funding models. Payers look for evidence of improved outcomes, cost savings, and better patient experiences. Policymakers weigh the potential benefits against upfront costs and training requirements, seeking assurances about safety, equity, and long term maintenance. Investment in workforce development is essential as therapists require new competencies to select appropriate devices, adjust settings, interpret data, and integrate robotics into holistic care plans. When public and private stakeholders collaborate to address these concerns, robotics can become a standard component of geriatric rehabilitation programs, accessible to diverse populations across different care settings and socioeconomic backgrounds.
Inspiring a future where technology honors the ageing journey
The trajectory of robotic assisted physical therapy points toward a future in which technology supports the aging journey with compassion, precision, and humanity. As robots learn to interpret musculoskeletal signals with increasing nuance, they will help clinicians design therapy that respects each person’s pace, preferences, and life story. The goal is not to automate care but to augment it in ways that elevate safety, sustain motivation, and expand the boundaries of what is possible for elders striving to maintain or reclaim their mobility and independence. The enduring message is one of partnership: between clinician and robot, between patient and program, and between health care institutions and the communities they serve. In that partnership, robotics becomes a quiet advocate for elderly well being, amplifying the virtues of tailored care, evidence informed practice, and the resilient human spirit that underlies every successful rehabilitation journey.
Closing reflections on integration, humanity, and ongoing innovation
As technology continues to evolve, the integration of robotics into elderly physical therapy invites ongoing reflection about how best to balance automation with personal presence. It invites therapists to imagine new ways to connect with patients, to translate complex data into meaningful conversations, and to design therapy that honors the full spectrum of aging experiences. The promise is not simply more efficient movement practice but a richer therapeutic alliance in which the robot serves as a facilitator for guided exploration, safe experimentation, and the gradual uncovering of capabilities that patients might not have believed possible. When implemented with care, thoughtful training, and a steady commitment to patient centered values, robotic assisted therapy can enrich the fabric of elder care, supporting not only physical recovery but the dignity, autonomy, and joy that are at the heart of meaningful aging.










