Understanding chronic kidney disease and why it matters
Chronic kidney disease is a long-term condition in which the kidneys gradually lose function, diminishing their ability to filter waste, balance fluids, and regulate minerals. When this process advances, wastes accumulate in the blood and can disrupt many body systems, leading to fatigue, fluid retention, and shifts in blood chemistry that require careful management.
CKD is identified by persistent reductions in kidney function or evidence of organ damage that lasts for three months or more. The most common measurements used in everyday care are an estimated glomerular filtration rate and the level of protein in the urine, both of which offer windows into how well the kidneys are performing.
Understanding CKD empowers patients to participate in decisions about treatment and lifestyle changes. Early attention to risk factors and regular monitoring can slow progression and protect heart health, bones, and the nervous system, improving overall wellbeing.
The impact of kidney disease extends beyond the kidneys themselves. It can influence energy levels, appetite, sleep quality, mood, and the ability to engage in daily routines. For many people, recognizing subtle warning signs early makes a meaningful difference in outcomes.
Causes and risk factors
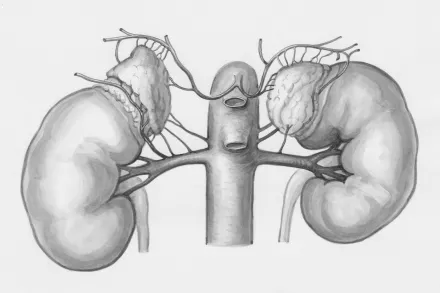
The two most common causes are diabetes and high blood pressure. Longstanding high blood sugar and sustained hypertension damage the tiny filtering units of the kidney, called nephrons, gradually eroding their capacity to clean the blood.
Other causes include inflammatory diseases that affect the kidney's filters, inherited conditions such as polycystic kidney disease, certain infections, kidney stones with chronic obstruction, and exposure to toxins or long-term use of particular medicines that harm renal tissue.
Risk factors that raise the chance of developing CKD include older age, a family history of kidney disease, obesity, smoking, and minority populations who may face higher rates of diabetes and hypertension. Social and economic factors also influence access to care and early detection.
In many cases CKD develops without noticeable symptoms for years, so people with diabetes, hypertension, or a family history should undergo regular screening rather than waiting for symptoms to appear. Early detection makes treatment more effective and can delay progression.
How CKD is diagnosed
Diagnosis begins with a clinician reviewing medical history, symptoms, and risk factors, followed by blood and urine tests to quantify kidney function and damage. Repeated measurements over months confirm that kidney problems are persistent rather than transient.
The estimated glomerular filtration rate is the standard gauge of kidney function. It is calculated from a blood creatinine value, age, sex, and other factors, and it classifies how well the kidneys filter waste from the blood.
Proteinuria, the presence of abnormal amounts of protein in the urine, signals damage to the kidney's filtering system. The degree of protein in the urine correlates with risk of progression and can influence treatment choices.
Additional tests such as electrolyte panels, anemia markers, bone mineral tests, imaging studies, and sometimes kidney biopsy help reveal the cause of injury and guide management strategies tailored to the individual patient.
Staging and progression
Chronic kidney disease stages range from 1 to 5, reflecting a combination of kidney function and evidence of organ damage. Stage 1 and 2 indicate normal or near-normal filtration with signs of damage, while stage 5 signifies kidney failure that may require replacement therapy.
Stage 3 is often subdivided into 3a and 3b to reflect mid-range function and rising risk. Stage 4 indicates more substantial loss of function, and stage 5 typically means the kidneys no longer meet the body's needs without intervention.
The pace of progression varies widely among individuals and depends on how well underlying diseases are controlled, the presence of other health problems, and lifestyle choices. Some people experience slow, gradual change over many years.
Staging informs planning for treatment, surveillance, and potential preparation for dialysis or transplantation. Regular monitoring helps detect acceleration in decline and prompts timely adjustments to therapy and goals.
Recognizing symptoms and warning signs
In the early stages CKD often presents no symptoms, which is why routine testing is crucial for at-risk individuals. When symptoms do appear, they may include fatigue, swelling in the ankles or abdomen, and changes in urination habits.
More advanced disease can bring persistent high blood pressure, bone or mineral metabolism problems, itchy skin, shortness of breath, and a general sense of being unwell. Some people notice sleep disturbances or difficulty concentrating as waste builds up in the body.
Because many symptoms are nonspecific, it is essential to discuss any new or ongoing concerns with a healthcare professional who can evaluate kidney function through blood and urine tests and assess related conditions such as anemia or electrolyte imbalances.
Early awareness does not replace medical care but it does prompt timely testing, which is why individuals with diabetes or hypertension should maintain regular checkups and ask about kidney screening when appropriate.
Key tests and measurements used in CKD care
The cornerstone tests include the estimated glomerular filtration rate and urine protein measurements. These two metrics provide a compact view of how well the kidneys work and the level of damage that has occurred.
Blood tests also monitor electrolytes, waste products such as creatinine and urea, and the balance of minerals like calcium and phosphorus. Abnormal values can signal the need to adjust medications or diet to protect bone health and heart function.
Additional assessments look at blood pressure control, anemia status, and markers of cardiovascular risk. Treating anemia, for instance, can improve energy, cognitive function, and quality of life while reducing heart strain.
Imaging studies such as ultrasound or other kidney imaging help visualize kidney size, structure, and potential obstructions. In selected cases a biopsy may be performed to identify the exact cause of kidney injury and tailor therapy accordingly.
Setting goals in CKD management
Careful goal setting centers on preserving remaining kidney function, managing symptoms, and preventing complications. Clinicians work with patients to define targets for blood pressure, glycemic control, and mineral balance that are realistic and evidence based.
Strategies emphasize slowing progression through the management of diabetes and hypertension, minimizing exposure to toxins, and ensuring adherence to therapies that have proven kidney benefits, such as certain classes of medications and lifestyle changes.
Patients are encouraged to engage in shared decision making, keeping preferences, daily routines, and cultural considerations in mind. Understanding risks and benefits of each option supports informed choices and ongoing motivation.
Because CKD is a chronic condition, goals are revisited regularly during clinic visits. Adjustments are common as kidney function evolves, symptoms change, and new treatments become available with meaningful evidence on outcomes.
Medications and how they help
Medications play multiple roles, from protecting kidney function to easing symptoms and reducing the risk of complications. Among the most important are drugs that lower blood pressure and reduce protein leakage into urine.
ACE inhibitors and ARBs are frequently prescribed for people with hypertension and kidney disease because they both lower pressure in delicate kidney vessels and lessen protein loss. Their protective effect can slow damage when used correctly.
Newer kidney friendly therapies include agents that improve metabolic health in diabetes and some cardiovascular drugs that provide kidney benefits beyond blood sugar or blood pressure control. These medications are chosen based on the patient’s profile and kidney stage.
Other medicines help manage anemia, phosphate balance, bone health, and electrolyte disturbances. Patients may also require iron supplements or vitamin D to maintain bone strength and energy levels when deficiencies are present, always under medical supervision to avoid dangerous interactions.
Diet and nutrition for kidney health
Nutrition supports kidney function by providing energy and nutrients while limiting substances that can threaten kidney health. Diet plans are personalized to stage, treatment plan, and coexisting conditions such as diabetes or heart disease.
Protein needs change with kidney function; too much protein can increase workload on the kidneys, while too little can lead to malnutrition. A careful balance helps preserve muscle mass and maintain overall health without accelerating damage.
Salt intake often requires reduction to help control blood pressure and reduce fluid retention. Potassium and phosphorus levels are also monitored, with adjustments based on lab results and dietary choices to prevent dangerous imbalances.
Hydration, calories, and nutrient timing are considered as part of a holistic plan. Patients are guided to choose foods rich in nutrients while avoiding highly processed items that carry excess sodium, sugar, or unhealthy fats.
Blood pressure, diabetes, and cardiovascular health
Maintaining blood pressure within a healthy range is central to CKD care because high pressures can damage the delicate filters of the kidneys and hasten decline. Lifestyle changes and medications work together to achieve targets.
Diabetes management is crucial since high blood sugar accelerates kidney injury. Interventions include monitoring glucose closely, adjusting medications, and protecting kidney function through agents with proven renal benefits.
Cardiovascular risk rises with CKD, making heart-healthy choices essential. That includes regular physical activity as tolerated, a balanced diet, smoking cessation, and prompt treatment of lipid disorders when indicated by clinicians.
Frequent follow-up and coordination among nephrologists, primary care providers, dietitians, and pharmacists help ensure medications, tests, and dietary plans stay aligned with kidney health goals and patient preferences.
Dialysis and kidney replacement therapy
Dialysis is a life sustaining treatment for people whose kidneys are no longer able to remove wastes effectively. Hemodialysis and peritoneal dialysis are the two main modalities, each with unique scheduling and benefits.
Hemodialysis typically involves sessions at a dialysis center several times per week, or in some cases at home, and it replaces a significant portion of kidney function during those treatments. The goal is to remove toxins and rebalance fluids consistently.
Peritoneal dialysis uses the body’s lining as a filter and can often be done at home, offering flexibility for daily life. Choice of modality depends on medical considerations, patient preference, and access to trained care teams.
Preparation for dialysis includes planning for vascular access, education, and social support. Early conversations about what to expect, how to manage complications, and how to maintain quality of life are important components of care.
Kidney transplantation and alternatives
Kidney transplantation offers a potential return to near-normal kidney function for many people with end-stage disease. A transplant can improve energy, independence, and overall well being compared with long term dialysis.
Donor options include living related or unrelated donors and deceased donor organs. The matching process considers tissue compatibility, blood type, and overall health to maximize transplant success and minimize rejection risk.
Immunosuppressive medications are essential after a transplant to prevent rejection. These drugs require ongoing monitoring and introduce considerations around infection risk and medication interactions, which teams manage through regular care.
For some patients transplantation may not be possible or desirable. Alternatives such as dialysis or conservative management focusing on quality of life can be chosen with careful discussion about goals and preferences, ensuring supportive care remains central.
Living with CKD: day-to-day life and mental health
Living with chronic kidney disease affects daily routines and energy levels. Planning ahead for medical appointments, medication schedules, and dietary restrictions can reduce stress and help maintain independence.
Emotional well being matters as much as physical health. Feelings of uncertainty, frustration, or isolation may emerge, and seeking support from counselors, support groups, or peers can provide practical strategies and comfort.
Activity can remain meaningful with adaptations. Gentle exercise, hobbies, and social connections support physical health, mobility, and mood while helping people stay engaged with life despite chronic disease.
Care coordination with a team that includes nephrologists, nurses, dietitians, social workers, and primary care providers ensures care is comprehensive. Open communication about symptoms, treatment burdens, and goals helps maintain quality of life.
Preventing progression and optimizing long-term outcomes
Preventing progression hinges on controlling diabetes and blood pressure, avoiding nephrotoxic substances, and adhering to medications proven to protect kidney function. Regular laboratory checks guide timely adjustments.
Avoiding dehydration and managing fluid balance are important, as is staying up to date on vaccines and infections to prevent illness that can destabilize kidney health.
Engagement with a multidisciplinary care team supports sustained gains. Dietitians, pharmacists, and social workers help tailor plans, review medications for interactions, and address practical barriers to care.
Empowerment comes from education, access to reliable information, and ongoing communication with clinicians. By staying informed and proactive, people can protect kidney health and maintain independence longer.
Staying informed and taking control of kidney health
The journey with CKD is highly individual, and knowledge is a powerful tool. Patients who understand testing results, potential side effects of treatments, and the rationale behind lifestyle changes can participate more fully in decisions.
Seeking second opinions, asking questions, and using trusted resources helps ensure care aligns with personal values and health goals. Regular communication with clinicians strengthens safety and confidence in care plans.
Family involvement and support networks play a critical role in adherence and emotional resilience. Sharing information with loved ones helps build an environment that supports healthy choices and timely action when problems arise.
With thoughtful planning and a proactive stance, people living with CKD can maintain meaningful activity, protect heart and bone health, and navigate treatments with greater clarity and calmness.










