Introduction to pancreatic health
The pancreas is a breadbasket of the digestive system, tucked behind the stomach and playing a dual role that is easy to misunderstand. On one side it produces digestive enzymes that are released into the small intestine to break down fats, proteins, and carbohydrates. On the other side it liberates hormones such as insulin that help regulate blood sugar levels. When either function is impaired by disease, the body may manifest a spectrum of symptoms, ranging from subtle changes in digestion to more dramatic signs like persistent pain or weight loss. Recognizing these signals can help people seek medical assessment promptly, which is especially important because pancreatic conditions can progress quietly before they become obvious. A careful attention to patterns of discomfort, changes in appetite, and alterations in bowel habits can make a meaningful difference in outcomes, guiding early diagnostic steps and treatment discussions with clinicians.
Understanding symptoms across pancreatic disorders
Symptoms linked to pancreatic disease are not always specific to a single condition and can overlap across disorders. Some indicators are shared by many pancreatic problems, including persistent upper abdominal discomfort, back pain, and a sense of fullness or heaviness after meals. Weight loss without an obvious cause, changes in appetite, and fatigue can accompany various pancreatic problems because the organ’s digestive role and its hormonal functions are deeply intertwined with overall energy balance and metabolism. If symptoms are new, persistent beyond a few weeks, or intensify despite basic self-care, medical evaluation becomes appropriate to determine whether the pancreas may be involved or if another condition is at play. It is important to keep in mind that sometimes early signs are mild or intermittent, which is why a pattern over time often matters more than a single episode.
Red flags for acute pancreatitis
One of the most urgent situations is acute pancreatitis, a sudden inflammation of the pancreas that can cause intense belly pain and systemic illness. The pain is frequently located in the upper abdomen and may radiate to the back, and it often worsens after meals or when lying supine. Accompanying symptoms can include nausea, vomiting, fever, a rapid pulse, and abdominal tenderness, and some people may develop swelling or a rigid abdomen. In addition to pain, dehydration and electrolyte disturbances can arise, demanding prompt medical attention. Recognizing these red flags early is crucial because acute pancreatitis can signal serious conditions such as gallstone obstruction or underlying pancreas injury, and timely treatment affects recovery and the prevention of complications.
Chronic pancreatitis and its ongoing signals
Chronic pancreatitis represents a longer-term inflammation of the pancreas that progressively damages the tissue and alters its ability to function. The pain associated with chronic pancreatitis is often persistent, though it may wax and wane, and it can be described as a deep ache or a burning sensation that travels to the back. Over time, people may notice meal-related discomfort, especially after fatty foods, and some experience a decrease in appetite or weight loss as digestion becomes less efficient. The diminished digestion leading to fat malabsorption can manifest as oily, pale stools that float and have a distinct, unpleasant odor. Fat-soluble vitamin deficiencies may emerge, contributing to fatigue, muscle weakness, or brittle bones if not addressed. The combination of chronic pain, digestive changes, and weight loss can be emotionally challenging as people adjust their routines around symptoms and treatment strategies.
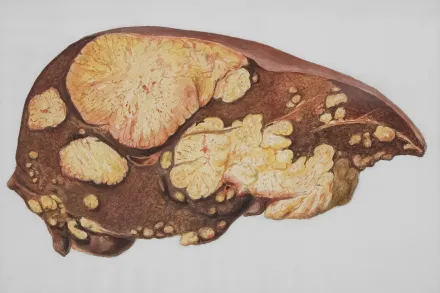
Pancreatic cancer warning signs
Pancreatic cancer often presents with a mix of signs that can appear gradually and may be subtle at first. Early symptoms can include jaundice, which gives the skin and whites of the eyes a yellow tint, dark urine, and pale stools that reflect bile flow obstruction. Unexplained, progressive weight loss accompanied by a reduced appetite and fatigue can also be noticeable. Some individuals report persistent upper abdominal or back pain that does not clearly align with meals or activity. Swelling or a palpable lump in the abdomen is less common but can occur in later stages. Because these symptoms can overlap with benign conditions, a clinician will typically evaluate personal risk factors and perform diagnostic tests to determine whether a growth or other pancreatic abnormality is present and to distinguish it from inflammatory processes.
Exocrine insufficiency and malabsorption signals
When pancreatic ductal function declines or the enzyme-producing cells are damaged, the body may struggle to digest fats and other nutrients. This exocrine insufficiency leads to greasy, foul-smelling stools that may float and be difficult to flush away, a sign that digestion is not happening efficiently. Weight loss without trying can accompany this malabsorption, and there may be general symptoms of nutrient deficiency such as hair loss, brittle nails, or a sense of fatigue that persists despite rest. Individuals who notice frequent abdominal cramps, bloating, or unusual stool changes after meals should consider a pancreas-focused evaluation, especially if these symptoms persist for several weeks. In some cases, fat-soluble vitamins A, D, E, and K may become depleted, producing additional symptoms like vision changes, bone tenderness, or easy bruising, which further support the need for professional assessment and possible digestive enzyme support.
New onset diabetes and pancreatic health
The pancreas also plays a central role in glucose regulation through insulin production. When pancreatic damage occurs, particularly in chronic disease or malignancy, the onset of diabetes can occur or existing diabetes may worsen. New-onset diabetes in adults, especially when accompanied by rapid weight loss or unusual fatigue, should prompt consideration of pancreatic disease as a contributing factor. Symptoms such as extreme thirst, frequent urination, blurred vision, and slowed wound healing are typical for diabetes but in the context of potential pancreatic disease they warrant careful evaluation to determine whether pancreatic dysfunction is involved or if there are additional metabolic issues requiring attention. Early recognition of this link can lead to timely diagnostic workups and targeted management that addresses both the pancreas and blood sugar control.
When to seek medical evaluation for pancreatic symptoms
Any persistent symptom related to digestion, abdominal pain, or unexplained weight loss warrants a careful medical check. If upper abdominal pain lasts more than a few days, is accompanied by fever, vomiting, dehydration, or a rapid heart rate, urgent assessment is appropriate as it may reflect an acute inflammatory process or another serious condition. Jaundice, dark urine, or pale stools changes should prompt prompt medical contact because of the possibility of bile duct obstruction or pancreatic tumor as potential causes. In addition, new onset diabetes symptoms in adults or rapid changes in appetite and weight that do not respond to conventional dietary adjustments should be evaluated to rule out underlying pancreatic problems. A clinician may guide a plan that includes history taking, physical examination, blood tests, imaging studies, and sometimes referral to a specialist for further evaluation.
How doctors evaluate symptoms and make a diagnosis
The evaluation of suspected pancreatic disease begins with a detailed history and a physical examination, focusing on the location, timing, and quality of pain, along with any associated digestive or metabolic signs. Laboratory tests commonly include measurements of pancreatic enzymes such as amylase and lipase, liver function tests, bilirubin, and blood glucose levels, as well as markers that may indicate malabsorption or nutritional deficiencies. Imaging studies play a central role, with ultrasound often used as an initial, noninvasive screen, and more detailed tests like computed tomography scans or magnetic resonance imaging providing a clearer view of pancreatic tissue, ducts, and surrounding structures. In some cases, specialized tests such as endoscopic ultrasound or MRCP are employed to assess ductal anatomy and detect small changes not visible on standard imaging. When a mass or suspicious lesion is found, tissue sampling through biopsy may be pursued to confirm a diagnosis. Stool tests may be ordered to quantify fat content and confirm exocrine insufficiency, while genetic testing might be considered for individuals with a strong family history or early onset forms of disease. The goal of these evaluations is to distinguish inflammation from cancer, assess the functional capacity of the pancreas, identify complications, and guide treatment decisions tailored to the patient’s specific condition and overall health.
Treatment considerations and symptom management
Management of pancreatic disease centers on alleviating symptoms, addressing the underlying cause, and preserving nutritional status. Pain control often requires a combination of medication, lifestyle adjustments, and sometimes procedures that relieve pressure within the pancreas or surrounding tissues. In cases of inflammatory disease, treating the trigger such as gallstones or severe alcohol use is essential, while for chronic conditions, long-term strategies focus on maintaining digestion with supplemental pancreatic enzymes and adjusting dietary fat intake to balance comfort with nutrition. When cancer is diagnosed, treatment planning depends on stage and patient factors, and may involve surgery, chemotherapy, radiation therapy, or targeted therapies until the disease is controlled or the goals of care are aligned with the patient’s preferences. Across all scenarios, maintaining hydration, controlling blood sugar as needed, and ensuring adequate nutrition are critical, as they support tolerance to treatments and overall quality of life even when symptoms persist. Patients often benefit from multidisciplinary teams that include physicians, dietitians, pain specialists, and mental health professionals to address both physical and emotional needs during the course of disease management.
Diet, lifestyle, and strategies to support pancreatic health
Although lifestyle changes alone cannot cure pancreatic disease, they can influence symptom severity and help protect general health. For digestive comfort and nutrient absorption, many clinicians recommend a balanced diet that emphasizes easily digested foods, adequate protein, and controlled fat intake, with adjustments based on tolerance and the degree of steatorrhea. Pancreatic enzyme replacement therapy is commonly used to aid digestion in people with exocrine insufficiency, helping to reduce symptoms such as greasy stools and weight loss while improving nutrient absorption. Maintaining proper hydration and a steady meal pattern can help stabilize digestion and energy levels. For individuals at risk of pancreatic disorders, avoiding tobacco products and limiting excessive alcohol intake are traditional preventive steps that may lower the likelihood of inflammatory or malignant processes. Regular physical activity, appropriate vaccination, and routine medical checkups further support overall health and facilitate early detection of any changes in pancreatic function, especially in individuals with a family history or predisposing risk factors.
Symptoms that may precede or accompany diabetes related to pancreatic disease
In some cases, pancreatic conditions may contribute to metabolic changes that manifest as altered glucose handling. People might notice an unusual increase in thirst, more frequent urination, and fatigue that does not fully result from sleep or stress. Blurred vision can accompany sustained high blood glucose, and slower wound healing is sometimes observed. While these signs are not exclusive to pancreatic disease, when they occur alongside digestive symptoms or weight changes, a clinician may pursue tests to evaluate pancreatic function, including assessments of insulin production, fasting glucose, and long-term glucose control. Early involvement of endocrinology or gastroenterology specialists can help ensure that both the digestive and metabolic aspects of pancreatic health are considered in the diagnostic and treatment plan.
Planning care and coordinating with specialists
Coordination of care becomes particularly important when multiple pancreatic conditions or complications are present. For patients with complex symptoms, a coordinated plan involving primary care providers, gastroenterologists, oncologists, pain specialists, and nutritionists helps address each facet of the disease. Communication about symptom patterns, response to treatments, nutritional status, and psychosocial concerns supports a more comprehensive approach. Education about medication timing, potential side effects, and the importance of adherence to enzyme supplements or insulin therapy can empower patients to participate actively in their own care. Emotional support, coping strategies, and access to patient resources are also valuable components of a holistic treatment strategy, helping individuals navigate the uncertainties that can accompany pancreatic disorders while maintaining dignity and independence wherever possible.
Prevention perspectives and ongoing risk assessment
Even for individuals who have never developed pancreatic disease, awareness of risk factors and healthy living habits can contribute to long-term pancreatic well-being. Maintaining a healthy body weight through balanced nutrition and regular physical activity can reduce the likelihood of inflammatory processes and certain cancers. Avoiding tobacco products, moderating alcohol consumption, and managing chronic conditions such as high triglycerides, high blood pressure, and diabetes itself are practical steps that have broad health benefits, including potential protective effects for the pancreas. Regular medical checkups, especially for those with a family history of pancreatic disease or known risk factors, enable clinicians to monitor for early signs, order appropriate tests when indicated, and initiate timely interventions that may slow progression or improve symptom control. A person who remains informed and engaged in their health care often experiences better outcomes and a greater sense of control over their pancreatic health journey.










